CBC Marketplace Consumer Mask Testing
Published: November 13th, 2020
Revised: February 23rd, 2023
Originally aired November 13 2020 on CBC Marketplace
Wearing a mask is critical to reducing the spread of COVID-19, but rigorous tests conducted on behalf of CBC’s Marketplace found that while some work very well, others offer little protection from the particles that transmit the novel coronavirus. One type of mask can even spread those particles to others
Sporometrics own Dr. James Scott joined the CBC Marketplace investigators to test out various types of masks based on materials, thickness, and whether masks with vents contained an added advantage. Find out which ones passed the test and which ones you should avoid using here
SARS-CoV-2, Environmental surfaces [COV-S]
Published: June 15th, 2020
Revised: March 21st, 2023
Why sample for COVID-19 in the indoor environment?
Limited recent study of surface viability of the COVID-19 virus indicates that it can remain detectable on different types of materials for several hours to days. According to the CDC, the COVID-19 viral RNA was detected for up to 17 days on surfaces within enclosed areas containing confirmed COVID-19 cases, such as the case on the Diamond Princess cruise ship. Given the persistence of this virus on surfaces, proper decontamination and disinfection strategies are of the utmost importance. In certain high-risk circumstances, monitoring for persistent viruses is the gold standard method for confirming the elimination of surface contamination of COVID-19.
How does the test work?
Our COVID-19 virus analysis is based on the Centers for Disease Control and Prevention, Respiratory Viruses Branch, Division of Viral Diseases protocol entitled 2019-NovelCoronavirus (2019-nCoV) Real-Time RT-PCR Diagnostic Panel, effective 15 March 2020 . We have adapted and validated these processes for environmental samples in consideration of our test equipment and consumables.
Quantitative Reverse Transcription PCR analysis (qRT-PCR) is a highly specific and sensitive tool for testing samples for a range of RNA-based biohazardous agents. For our COVID-19 virus test, results will be reported as Positive or Not Detected. It is important to note that environmental RNA is highly unstable. SARS-CoV-2 consists of an RNA genome contained in a shell-like protein nucleocapsid which, in turn, is tucked inside an envelope composed of human cell membrane – this envelope protects the viral RNA from the environment. Once the integrity of the outer membrane is breached, environmentally abundant RNA-degrading enzymes rapidly destroy the viral RNA. Thus a positive result from this test is considered confirmatory of the presence of intact, infective virus particles.
Environmental Surface Sampling for COVID-19
Surface sampling procedures for the COVID-19 agent are described in the World Health Organization protocol entitled Surface sampling of coronavirus disease (COVID-19): Apractical “how to” protocol for health care and public health professionals dated February 18, 2020. This protocol should be followed when developing a post-decontamination sampling plan and collecting samples for submission for COVID-19 virus analysis.
Sporometrics-provided swabs for COVID-19 analysis will only be accepted. Swabs used for bacterial or fungal testing do not provide the same efficiency of viral RNA recovery and should not be used or submitted for this purpose. Decisions involving results and nonconformity of samples are the client’s responsibility. It is important to note that the swabs provided to you by Sporometrics are not the nasopharyngeal swabs used for clinical testing. Sporometrics understands the importance of maintaining the supply chain for our hospitals and healthcare industry.
For more information, please contact Sporometrics and a representative will be available to assist you.
Submission Instructions
Please contact Sporometrics prior to submitting any samples for COVID-19 virus testing. We will send you a work order with pricing and terms and conditions to sign and return. Sporometrics will provide test collection kits containing swabs and sampling instructions. It is critical that all samples are collected and submitted in accordance to our protocols, for protection of our team’s health and safety as well as your own.
Our AIHA Laboratory Accreditation Programs scope includes RT-PCR Covid-19 analyses for environmental air and swab samples.
Laboratory code: COV-S
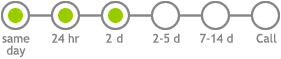
Service options
Related
SARS-CoV-2, Air [COV-A]
Published: May 26th, 2020
Revised: March 21st, 2023
SARS-CoV-2 transmission
The COVID-19 virus is mainly thought to be transmitted between people through large respiratory droplets during close contact, and is not generally thought to move greater distances on fine particles (1). Aerosols arising from the respiratory tract are often distinguished as either droplets or airborne particles. This categorical distinction is arbitrary, and instead these two groupings merely represent conceptual prototypes of a more complex set of intergrading phenomena.
All aerosols emitted from the respiratory tract begin their journey as liquid droplets additionally containing non-liquid items, such as epithelial cells, bacterial cells and virus particles. Immediately when these droplets are released the water in them begins to evaporate as long as the relative humidity (RH) of the ambient air is below saturation.
Droplet nuclei
For example, in air of 80% RH, the liquid in a small droplet of 1 micrometer in diameter evaporates completely within 5 milliseconds, and this droplet becomes a dust particle which remains aloft in the air because of its very small size. Under similar conditions, a droplet of 10 micrometers in diameter loses all of its liquid water after one third of a second, leaving behind a dust particle of reduced in size (e.g., 50-75% smaller, roughly 2.5 to 5 micrometers in diameter) that contains all of the solid materials present in the original droplet. Like its tinier cousin, this larger particle is also very buoyant in air, falling under force of gravity at a rate of only 1-5 centimeters per minute. By contrast, larger liquid droplets such as those 100 micrometers in diameter, are subject to gravitational forces to a much greater extent, falling initially at a rate of about 30 centimeters per second. These larger droplets fall so swiftly that they lack sufficient time (>14 seconds, roughly half a meter of descent) to evaporate and become smaller, loftier particles before they collide with surfaces while still liquid ( 2).
Virions of SARS-CoV-2 themselves are very tiny, on the order of 100 nanometers in diameter. They are only emitted in droplets of the size ranges described above. Inside these droplets, virions can be packed like gumballs in a gumball machine. The larger the droplet, the greater its ability to contain infective virus. For droplets larger than the size of the virus itself, the physical volume of a droplet to contain virions scales as a cubic function of its diameter. A droplet of 10 micrometers can contain no more than 370 or so virions, whereas a droplet of 10 micrometers can contain 370,000. Thus, larger droplets have far greater potential to carry a viral burden ( 2).
The question, then, of whether a particular virus is spread by “droplets” or ”airborne particles” is fundamentally a composite question of how virulent the agent is and how dense the particle field is likely to be. As far as SARS-CoV-2 is concerned, we know that it is far less contagious than measles virus, where only a single virion is able to cause disease. To cause a SARS-CoV-2 infection, at least 1,000,000 virions or more are probably needed. This is a number that potentially could be carried in a single large droplet of 100 micrometers in diameter. But multiple smaller dust particles, such as those described above may also be sufficient (e.g., > 3 particles that began as 10 micrometer diameter droplets, or 3,000 that began as 1 micrometer droplets). Thus the density of particles in the air (and the persistence of their infectivity) is the major determinant of whether this virus can be transmitted by airborne particles or droplets, or a combination.
Environmental propagation pathways
In addition to respiratory secretions, it is becoming increasingly clear that SARS-CoV-2, like its cousin SARS-CoV-1 responsible for the 2002–2003 outbreak in south China, can be present in vomitus and feces ( 3). The act of flushing a toilet containing containing infected feces can aerosolize significant concentrations of airborne viruses ( 4, 5). Depending on the size of the particles remaining after the liquid has evaporated, virus can remain airborne for lengthy periods, resulting in exposure and infection. Spread of infectious particles through by mechanical systems is thought to be a major cause for the rapid spread of SARS in the Amoy Plaza Hotel in Hong Kong in February 2003 ( 3).
The possibility of airborne transmission has become a real concern, that the World Health Organization (WHO), has updated their infection control measures to implement “airborne precautions” for all medical staff (1).
Why sample for SARS-CoV-2 in the environment?
A small but growing number of scientific publications have shown that SARS-CoV-2 can be found in the indoor environment. It has been suggested that the virus can remain viable in aerosols for up to 3 hours ( 6). Airborne SARS-CoC-2 particles have been routinely detected in areas where there are confirmed cases (such as in health care settings), and in some instances the transmission distance in the air is thought to be up to 4 meters ( 4, 5, 7).
As many office and retail buildings prepare to reopen, proper infection control practices to date mainly focus on transmission through close contact and surface transmission. It is equally important to consider implementing measures to reduce viral transmission through aerosols.
To this end we must consider the following:
- What engineering controls may be applied to minimize the spread of bioaerosols?
- How effective are the current building engineering controls?
According to the WHO, adequate ventilation in all patient-care areas is necessary to help prevent airborne infections. The overall airflow should bring the air from contaminated sources to areas where there is sufficient dilution, and preferably to the outdoors (8). Ventilation and filtration provided by heating, ventilating, and air-conditioning systems that employ high-efficiency particulate air filters (HEPA) for particle filtration have been shown to remove such virus-laden aerosols (9).
Air sampling may be conducted to determine indoor air quality and can give assurance of proper ventilation. The CDC considers air sampling as a practical method for evaluating the infection-control performance of the HVAC system, with an emphasis on filter efficiency in removing respirable particles or larger particles from the air (10).
Our AIHA Laboratory Accreditation Programs scope includes RT-PCR Covid-19 analyses for environmental air and swab samples.
How to sample air for SARS-CoV-2
Sporometrics can conduct our RT-PCR analysis for SARS-CoV-2 on air samples collected by a few methods including dry cyclone, 37 mm endotoxin-free cassette with 0.4 µm Polycarbonate Filter, and PTFE 0.3 µm, 37 mm filters.
Submission Instructions
Please contact Sporometrics prior to submitting any samples for COVID-19 virus testing. We will send you a work order with pricing and terms and conditions to sign and return. Sporometrics will provide guidance on sampling supplies and sampling instructions. It is critical that all samples are collected and submitted in accordance to our protocols, for protection of our team’s health and safety as well as your own.
If you are interested in using a different sampling method or would like more information on air sampling of viral particles, please contact Sporometrics.
Laboratory code: COV-A
Service options
Related
SARS-CoV-2 (COVID-19 virus) Analysis
Published: April 16th, 2020
Revised: March 19th, 2025
Sporometrics is proud to offer analysis services by RT-PCR for SARS-CoV-2, the virus responsible for COVID-19. The purpose of this analysis is to support our clients by providing confidence in the effectiveness of decontamination activities and minimize exposure risk during this challenging period. (more…)
Surveys reveal a complex association of phytoplasmas and viruses with the blueberry stunt disease on Canadian blueberry farms
Published: April 9th, 2019
Revised: April 9th, 2019
Surveys for phytoplasmas and viruses were conducted during September 2014 and 2015 on highbush blueberry farms in the Région Montérégie, Quebec. Total DNA and RNA were extracted from blueberry bushes showing blueberry stunt (BBS) symptoms and from symptomless blueberry bushes, and utilised as templates for PCR and RT‐PCR assays, respectively. Phytoplasma DNA was amplified with universal phytoplasma primers that target the 16S rRNA, secA and secY genes from 12 out of 40 (30%) plants tested. Based on 16S rRNA, secA and secY gene sequence identity, phylogenetic clustering, actual and in silico RFLP analyses, phytoplasma strains associated with BBS disease in Quebec were identified as ‘Candidatus Phytoplasma asteris’‐related strains, closely related to the BBS Michigan phytoplasma strain (16SrI‐E). The secY gene sequence‐based single nucleotide polymorphism analysis revealed that one of the BBS phytoplasma strains associated with a leaf marginal yellowing is a secY‐I RFLP variant of the subgroup 16SrI‐E. Two viruses were detected in blueberry bushes. The Blueberry Red Ringspot Virus (BRRV) was found in a single infection in the cultivar Bluecrop with no apparent typical BRRV symptoms. The Tobacco Ringspot Virus (TRSV) was found singly infecting blueberry plants and co‐infecting a BBS phytoplasma‐infected blueberry cv. Bluecrop plant. This is the first report of TRSV in the cv. Bluecrop in Quebec. The Quebec BBS phytoplasma strain was identified in the leafhopper Graphocephala fennahi, which suggests that G. fennahi may be a potential vector for the BBS phytoplasma. The BBS disease shows a complex aetiology and epidemiology; therefore, prompt actions must be developed to support focused BBS integrated management strategies.