SARS-CoV-2, Air [COV-A]
Published: May 26th, 2020
Revised: March 21st, 2023
SARS-CoV-2 transmission
The COVID-19 virus is mainly thought to be transmitted between people through large respiratory droplets during close contact, and is not generally thought to move greater distances on fine particles (1). Aerosols arising from the respiratory tract are often distinguished as either droplets or airborne particles. This categorical distinction is arbitrary, and instead these two groupings merely represent conceptual prototypes of a more complex set of intergrading phenomena.
All aerosols emitted from the respiratory tract begin their journey as liquid droplets additionally containing non-liquid items, such as epithelial cells, bacterial cells and virus particles. Immediately when these droplets are released the water in them begins to evaporate as long as the relative humidity (RH) of the ambient air is below saturation.
Droplet nuclei
For example, in air of 80% RH, the liquid in a small droplet of 1 micrometer in diameter evaporates completely within 5 milliseconds, and this droplet becomes a dust particle which remains aloft in the air because of its very small size. Under similar conditions, a droplet of 10 micrometers in diameter loses all of its liquid water after one third of a second, leaving behind a dust particle of reduced in size (e.g., 50-75% smaller, roughly 2.5 to 5 micrometers in diameter) that contains all of the solid materials present in the original droplet. Like its tinier cousin, this larger particle is also very buoyant in air, falling under force of gravity at a rate of only 1-5 centimeters per minute. By contrast, larger liquid droplets such as those 100 micrometers in diameter, are subject to gravitational forces to a much greater extent, falling initially at a rate of about 30 centimeters per second. These larger droplets fall so swiftly that they lack sufficient time (>14 seconds, roughly half a meter of descent) to evaporate and become smaller, loftier particles before they collide with surfaces while still liquid ( 2).
Virions of SARS-CoV-2 themselves are very tiny, on the order of 100 nanometers in diameter. They are only emitted in droplets of the size ranges described above. Inside these droplets, virions can be packed like gumballs in a gumball machine. The larger the droplet, the greater its ability to contain infective virus. For droplets larger than the size of the virus itself, the physical volume of a droplet to contain virions scales as a cubic function of its diameter. A droplet of 10 micrometers can contain no more than 370 or so virions, whereas a droplet of 10 micrometers can contain 370,000. Thus, larger droplets have far greater potential to carry a viral burden ( 2).
The question, then, of whether a particular virus is spread by “droplets” or ”airborne particles” is fundamentally a composite question of how virulent the agent is and how dense the particle field is likely to be. As far as SARS-CoV-2 is concerned, we know that it is far less contagious than measles virus, where only a single virion is able to cause disease. To cause a SARS-CoV-2 infection, at least 1,000,000 virions or more are probably needed. This is a number that potentially could be carried in a single large droplet of 100 micrometers in diameter. But multiple smaller dust particles, such as those described above may also be sufficient (e.g., > 3 particles that began as 10 micrometer diameter droplets, or 3,000 that began as 1 micrometer droplets). Thus the density of particles in the air (and the persistence of their infectivity) is the major determinant of whether this virus can be transmitted by airborne particles or droplets, or a combination.
Environmental propagation pathways
In addition to respiratory secretions, it is becoming increasingly clear that SARS-CoV-2, like its cousin SARS-CoV-1 responsible for the 2002–2003 outbreak in south China, can be present in vomitus and feces ( 3). The act of flushing a toilet containing containing infected feces can aerosolize significant concentrations of airborne viruses ( 4, 5). Depending on the size of the particles remaining after the liquid has evaporated, virus can remain airborne for lengthy periods, resulting in exposure and infection. Spread of infectious particles through by mechanical systems is thought to be a major cause for the rapid spread of SARS in the Amoy Plaza Hotel in Hong Kong in February 2003 ( 3).
The possibility of airborne transmission has become a real concern, that the World Health Organization (WHO), has updated their infection control measures to implement “airborne precautions” for all medical staff (1).
Why sample for SARS-CoV-2 in the environment?
A small but growing number of scientific publications have shown that SARS-CoV-2 can be found in the indoor environment. It has been suggested that the virus can remain viable in aerosols for up to 3 hours ( 6). Airborne SARS-CoC-2 particles have been routinely detected in areas where there are confirmed cases (such as in health care settings), and in some instances the transmission distance in the air is thought to be up to 4 meters ( 4, 5, 7).
As many office and retail buildings prepare to reopen, proper infection control practices to date mainly focus on transmission through close contact and surface transmission. It is equally important to consider implementing measures to reduce viral transmission through aerosols.
To this end we must consider the following:
- What engineering controls may be applied to minimize the spread of bioaerosols?
- How effective are the current building engineering controls?
According to the WHO, adequate ventilation in all patient-care areas is necessary to help prevent airborne infections. The overall airflow should bring the air from contaminated sources to areas where there is sufficient dilution, and preferably to the outdoors (8). Ventilation and filtration provided by heating, ventilating, and air-conditioning systems that employ high-efficiency particulate air filters (HEPA) for particle filtration have been shown to remove such virus-laden aerosols (9).
Air sampling may be conducted to determine indoor air quality and can give assurance of proper ventilation. The CDC considers air sampling as a practical method for evaluating the infection-control performance of the HVAC system, with an emphasis on filter efficiency in removing respirable particles or larger particles from the air (10).
Our AIHA Laboratory Accreditation Programs scope includes RT-PCR Covid-19 analyses for environmental air and swab samples.
How to sample air for SARS-CoV-2
Sporometrics can conduct our RT-PCR analysis for SARS-CoV-2 on air samples collected by a few methods including dry cyclone, 37 mm endotoxin-free cassette with 0.4 µm Polycarbonate Filter, and PTFE 0.3 µm, 37 mm filters.
Submission Instructions
Please contact Sporometrics prior to submitting any samples for COVID-19 virus testing. We will send you a work order with pricing and terms and conditions to sign and return. Sporometrics will provide guidance on sampling supplies and sampling instructions. It is critical that all samples are collected and submitted in accordance to our protocols, for protection of our team’s health and safety as well as your own.
If you are interested in using a different sampling method or would like more information on air sampling of viral particles, please contact Sporometrics.
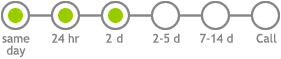
Laboratory code: COV-A
Service options