Total aerobic microbial count [TAMC]
Published: March 21st, 2023
Revised: March 21st, 2023
This test measures total culturable bacteria contained in a sample of pharmaceutical product, personal care product, medical device, of other similar material by culturing a measured amount of the sample on Tryptic Soy Agar and incubating at 30-35°C for a minimum of 3 days prior to analysis. At the end of the incubation period, bacterial colonies are counted and reported as CFU/g or CFU/mL. This test is usually conducted on bulk/ fluid samples, but it can also be used to test air.
Laboratory code: TAMC
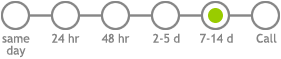
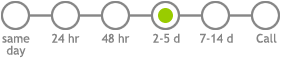
Service options
Pseudomonas aeruginosa culture [PSEUDO]
Published: March 21st, 2023
Revised: March 21st, 2023
Background
The Gram negative bacterium Pseudomonas aeruginosa is commonly found in soil, water, and other natural environments. It is an opportunistic pathogen that can cause infections in humans, particularly in individuals with weakened immune systems, such as those with cystic fibrosis or hospitalized patients. P. aeruginosa is known for its ability to form biofilms, which makes it difficult to treat with antibiotics. It is also resistant to many commonly used antibiotics, which can make infections difficult to treat. P. aeruginosa is a versatile organism that can thrive in a variety of environments and can cause a range of infections, from skin infections to pneumonia and sepsis.
Analysis
This test uses a semi-selective growth medium (Cetrimide Select agar) to detect and culture and differentiate P. aeruginosa from water samples. Results of this test are reported quantitatively as CFUs of P. aeruginosa per 100 mL.
Sample collection procedure
- Collect 500 mL of water in clean, new, screw-top bottle. For water sources expected to contain disinfectant chemicals such as chlorine, the collection container should include a suitable preservation buffer if biocides are likely to be present (the US-CDC recommends sodium thiosulfate to a final concentration of 0.1 M). We are pleased to provide sample collection containers to meet your needs. Please contact us prior to sampling to make arrangements.
- Transport samples to the laboratory as soon as possible after collection. Samples may be transported at room temperature but must be protected from temperature extremes. Samples not processed with 24 hours of collection must be refrigerated.
Laboratory code: PSEUDO
Service options
E. coli & coliforms, quantitative [ECOLI-Q]
Published: March 21st, 2023
Revised: March 21st, 2023
Coliform bacteria are common environmental bacteria, typically associated with the mammalian digestive tract. Although not generally pathogenic themselves, coliforms are a well-known marker of fecal contamination, and their presence is interpreted to suggest that potentially pathogenic bacteria may be present.
This test detects both E. coli and coliform bacteria in bulk water samples or from surfaces where the collection area is known. The test is adapted from the Health Canada method used to evaluate recreational water quality. Testing for E. coli and coliform bacteria together increases the analytical specificity of the test, and reduces the potential for false positive results.
This test uses a special growth medium for coliform bacteria that is incubated for a minimum of 48 hr prior to analysis, and enumerates total coliforms, parting out E. coli specifically. The number of colonies per plate or strip is enumerated, and the result is normally expressed quantitatively depending on the sample matrix (e.g., CFU/mL, CFU/100cm2, CFU/g, etc.). Please note, we are unable to perform this test for the purpose of assessing drinking water potability. This test is normally conducted from a liquid water sample or a swab collected from a defined surface area.
Laboratory code: ECOLI-Q
Service options
Legionella pneumophila culture with serotyping [LPC]
Published: March 3rd, 2023
Revised: March 3rd, 2023
Background
The Gram negative bacterium Legionella pneumophila is a common environmental cause of pneumonia, often associated with institutional outbreaks and environmental exposures. Legionella pneumophila is an endosymbiont of single celled protozoa that live in warm, stagnant water, particularly around temperatures of 30-40 °C. Building systems such as humidifiers and evaporative coolers may become contaminated by Legionella species including L. pneumophila if maintenance practices lapse or in the event of mechanical failures. Certain types of domestic hot water systems may also become affected. Most susceptible are systems in which untreated cold water is mixed with hot water downstream of the heating unit, usually as a means to prevent scalding at the faucet.
Analysis
This test uses selective and semi-selective culture-based assays recommended by the US-CDC to detect and differentiate culturable Legionella pneumophila Serotype 1 from Serotypes 2-15 in water and swab samples using a combination of physiological and immunological testing. Results of this test are reported quantiatively as CFUs of Legionella pneumophila Serotype 1 and L. pneumophila Serotype 2-15 (combined) per mL, or rated semi-quantitatively on swabs. For a more rapid species-specific test (24-48 hr), consider our molecular genetic Legionella pneumophila qPCR screen [M205]. Where L. pneumophila needs to be identified and enumerated specifically but serotyping is not required, consider Legionella pneumophila culture screen [C241].
Sample collection procedure
- Collect 500 mL of water in clean, new, screw-top bottle. For water sources expected to contain disinfectant chemicals such as chlorine, the collection container should include a suitable preservation buffer (the US-CDC recommends sodium thiosulfate to a final concentration of 0.1 M). We are pleased to provide sample collection containers to meet your needs. Please contact us prior to sampling to make arrangements.
- Collect culture swabs of internal surfaces of faucets, aerators, and shower heads using a sterile swab with buffered charcoal transport medium.
- Transport samples to the laboratory as soon as possible after collection. Samples may be transported at room temperature but must be protected from temperature extremes. Samples not processed with 24 hours of collection must be refrigerated.
References
- American Public Health Association. 2007. 9260 Detection of Pathogenic Bacteria: Section J – Legionella. APHA Standard Methods, Washington DC.
- Barbaree JM, Gorman GW, Martin, WT, Fields, BS, Morrill WE. 1987. Protocol for sampling environmental sites for legionellae. Appl Environ Microbiol 53: 1454-1458.
- Fields BS. 2006. Legionella, Chapter 79. In: Manual of Environmental Microbiology, 3rd edition. Hurst CJ, Crawford RL, Garland JL, Lipson DA, Mills AL, Stetzenbach LD (eds). Washington DC: American Society for Microbiology Press.
- US-CDC. 1992. Procedures for the recovery of Legionella from the environment. Atlanta GA : US Department of Health and Human Services, Public Health Service, 1-13.
Laboratory code: LPC
Service options